Leveraging analytics for effective Stars management
August 01, 2019
The success of MA health plans has become rooted in the ability to outperform the competition in terms of price and quality. This reality has placed pressure on achieving a coveted 4 or 5 Star rating. For the 40%-44% of plans who do succeed, they are rewarded with $25 to $34 PMPM, which is then reinvested in the plan to reduce prices and increase quality. It does not come as a surprise that while there is some variation in plans that achieve 4 Stars year-over-year, those that reach 5 Stars are relatively fixed and are generally provider-based local plans. For plans trying to break into the top 40%, an effective approach must be put in place to overcome the challenges of reaching 4+ Stars.
Regardless of a plan’s Star rating, certain challenges, both external and internal, are widening the gap between Star scores. Top performing plans are raising Star benchmarks each year and placing downward pressure on product pricing. Meanwhile, access to accurate and timely data from provider networks remains difficult to extract. Further exacerbating these challenges, we have seen plans struggle to optimize their operations and leverage data to inform targeted strategies that indicate whom to engage, with what content and through which channel.
To help a 3-Star plan that had lost 25% of its Medicare Advantage membership, was swamped by operational complexities and hindered by limited insights, launch a new and successful approach to 4 Stars, we leveraged our observations of 4+ Star plans from across the country.

What challenges should plans overcome to reach 4+ Stars?
After repeated declines in their Star ratings, the plan’s leaders were keen to understand what they could do to propel them to the next Star level. Our observations led us to conclude that certain foundational capabilities are critical in addressing common challenges.
Shift from targeting providers and members unanimously to segmenting and prioritizing groups
Health plans need to engage with members and providers in meaningful ways to deliver the right information to the right individuals. In order to accomplish this, a continuous segmentation process must be conducted that prioritizes members and providers based on characteristics, such as open care gaps and Stars performance. Once members and providers are properly segmented, information can be tailored to their needs and delivered through the right mix of digital and traditional channels.
Turn generalized incentives into ones that align provider and member interests to those of the plan
Incentives for gap closures have proven to be powerful tools to improve Stars outcomes. Working as signals, incentives not only indicate the value of a certain health activity but also encourage their audience to complete it. Therefore, it is critical to leverage insights that indicate the right amount of an incentive to drive the desired activity.
Move from generic to personalized care, providing information where, when and how the member needs it
Leading plans are leveraging member data to provide personalized content that helps members make important health decisions and close care gaps. The most advanced plans are also using analytics to proactively engage with members through their preferred channel: mobile, print, web or retail store.
Refine fragmented data collection and reporting to be a streamlined and accurate process
To impact highly weighted clinical measures, setting up a constant stream of data from providers has shown to improve results. The first step involves optimizing data delivery: data is sent in a consistent format from all participating providers, delivered on a set cadence, and stored in a location that is accessible to all relevant parts of the enterprise. The second step includes translating data into provider-specific gaps-in-care reports, highlighting actionable insights at the member-level, and sending reports in a timely fashion to providers.
Shift traditional mentalities towards a data-driven culture
The keystone off all Stars related efforts lies in a payor’s ability to continuously evaluate its performance. This necessitates the constant tracking of measures and the programs that impact them. This enables payors see the results of their efforts, re-prioritize their focus areas and understand the levers they can pull to drive better outcomes.
How are plans getting there?
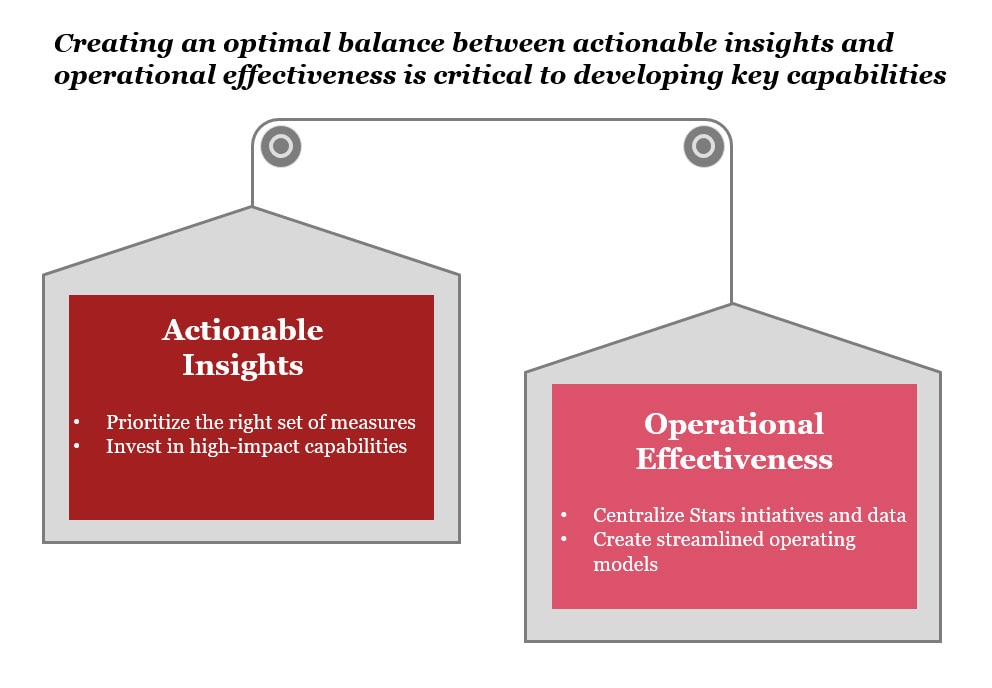
To develop these foundational capabilities, leading payers have leveraged inorganic and organic strategies. Plans that choose “inorganic” strategies acquire provider groups to increase their control of care delivery or purchase a higher performing plan to boost star ratings and capitalize on better processes. For this plan, the leaders chose to embark on the alternative “organic” approach to drive star ratings. They embarked on developing these key capabilities upon two pillars. One was actionable insights and the other was operational effectiveness. Their focus is now to create the optimal balance between the two.
Data driven decision support to turn insights to action
Gut instinct or “hunches” are no longer sufficient in making business decisions. To truly succeed and achieve higher Star ratings, plans need to leverage their data to uncover insights that business leaders and managers can use to make informed decisions. The first step in a data-driven Stars strategy is to prioritize a set of measures that will drive the plan to a higher Star rating. These measures are those which the payor has the greatest probability of influencing and have the greatest impact on the overall Star score. As a plan’s Stars performance changes throughout the year, so too will the predictive model used to prioritize measures. Therefore, measures should be evaluated on a normal cadence.
Once the prioritization has been set, the plan must invest in programs and capabilities that have the highest impact on the key measures. To best implement these programs, insights must be generated to answer key questions about program operations. Which member and/or providers should be targeted? How frequently should they be engaged? What channels should be leveraged? What the program’s impact on gap closure rates? These insights will enable program managers to make in-flight adjustments that ultimately result in higher Star scores.
Centralized Stars operations
The critical link between deriving these insights and turning them into actions is a collaborative and streamlined operating model. Best in class plans are now adopting a Stars Command Center that centralizes all Stars initiatives and data under one roof. This provides plans with greater control over all enterprise-wide Stars initiatives, provides a single view into Stars performance, fosters cross-functional collaboration, and allows leaders to offer guidance and support to their team members in optimizing program design and delivery.
Reaching a 4+ Star rating is a continuously moving target and executives across health plans must look to an innovative approach to overcome challenges to success. To head off challenges, they can turn to a two-pronged approach that balances data-driven insights and operational efficiencies to fortify foundational capabilities and drive Star ratings.
Contact us



Contact us



