Today’s healthcare landscape is yearning for the power of digital health
As discussed in our previous article (Decoding digital health: A success story for pharma?), we live in an era where healthcare systems worldwide are confronted with unprecedented challenges, and finding sustainable and innovative solutions is imperative. Over the last decade, healthcare expenditure has surged by a staggering 24% across the EU, according to the European Commission's 2022 report. Furthermore, a significant 35.2% of people in the EU are living with chronic health problems, underscoring the urgent need for transformative approaches1.
What is digital health and why does it matter?
As pharmaceutical companies (PharmaCos) navigate this landscape, digital health solutions (DHS) are emerging as transformative tools, offering the promise of enhanced patient outcomes and streamlined healthcare delivery. DHS represents a groundbreaking fusion of information and communications technologies within the medicine and healthcare professions, and incorporates the use of digital tools such as telemedicine, remote monitoring, health platforms, and apps, all aimed at managing illnesses, mitigating health risks, and promoting wellness.
Healthcare stakeholders eagerly embrace digital health solutions
Triggered by the Covid pandemic, global venture investors poured a record-breaking $51.9 billion into the field in 20212. While investments have fallen through to Q3 2023, funding for other industries has fallen even more strongly – the pharmaceutical and life sciences industries are faring better than others in terms of funding and outlook3. Overall, this represents an overdue correction, during global economic uncertainty across industries.

Over recent years, patients and healthcare professionals are becoming increasingly digital. Statista predicts a staggering 18.2 billion mobile devices by 2025, and in the EU 55% of individuals aged 16 to 74 sought health-related information online in Q1 20204. On the healthcare provider HCP side, the OECD concludes that 93% of primary care practitioners in 24 countries are now using digital technologies, such as electronic medical records (EMRs). As PharmaCos continue to search for opportunities to reduce costs (e.g., to cut spend per drug approval) and for novel approaches to therapeutics and diagnostics (e.g., via the mobile phone), partnering with digital health solutions or developing such solutions themselves seems promising.
However, as outlined in our previous article (Decoding digital health: A success story for pharma?), there are still many prominent examples of failure, such as Proteus Digital Health, which gained regulatory approval for the first 'smart pill' in the U.S. in 2017 but faced market challenges and lost a development deal with Otsuka Pharmaceuticals. Novartis' Sandoz also withdrew from a prescription app deal with Pear Therapeutics, and Sanofi scaled back its three-year-old partnership with Verily and their virtual diabetes clinic, Onduo.
Overall, PharmaCos need strategic vision and innovation to navigate the DHS journey successfully. Drawing on our expertise, we provide a brief guide highlighting five critical aspects.
Recommended reading
Decoding digital health: A success story for pharma?
Why do PharmaCos that strive to develop DHS often fail in doing so?
While the reasons are manifold, the top five that we observe are the following:
-
1Failing to design a user-centric DHS
A huge challenge lies in the art of crafting a user-centered DHS design. The failure to engage end-users in co-development often leads to a mismatch between the solution and the market. Implementations of DHS frequently face rejection due to their inability to effectively address the complex needs of patients, caregivers, and healthcare professionals. Issues such as poor integration into existing workflows, limited adaptability in cross-sector settings, insufficient value propositions, and absent key features are common pitfalls.
-
2Struggling with the partnership puzzle in DHS
Effective partnerships are the foundation of successful DHS ventures. Yet, forging alliances within the digital health sphere requires nuanced understanding. The absence of strategic collaborations, or alignment with incongruent entities, can be detrimental. Development teams, engrossed in the product, might overlook the vital ecosystem around it. Misalignments, transparency gaps, and wavering commitment can thwart validation efforts and hinder the solution's launch.
-
3Losing the PharmaCo neutrality balancing act
PharmaCos are drawn to the potential of integrating a popular DHS implementation into their portfolios. However, the challenge lies in balancing trust and transparency. Branding a digital health solution through a PharmaCo lens can raise questions about its primary beneficiary, potentially eroding trust. Striking the right balance between promotion and a genuinely patient-centric focus is crucial.
-
4Lacking validation of the business model
Most DHS-oriented businesses fail within their first few years – and yet more are not even launched successfully. Business model validation in the realm of DHS is a complex endeavor. Many promising solutions stumble due to a lack of rigorous business model validation throughout the development journey. As mentioned in our previous article, the revenue dimension specifically - particularly navigating reimbursement complexity and assessing willingness to pay - often remains problematic. Failure to unravel these nuances can ultimately lead to the solution being discontinued.
-
5Cracking the core of a strong DHS data strategy
In DHS development, one of the critical components often overlooked is a robust data strategy. The data requirements and value proposition, both for PharmaCos and other stakeholders, frequently defy comprehensive planning. IoT devices, despite their potential, often face resistance from healthcare professionals due to unreliable data collection and analysis methods, highlighting the importance of a trustworthy data strategy. Other challenges we observe include, amongst others, poor technical integration with existing (healthcare) systems and user workflows, inadequate data privacy and security, limited scalability and adaptability, resistance from healthcare professionals, a lack of regulatory and compliance research/work, and insufficient market research. For more detailed insights, please also refer to our previous article (Decoding digital health: A success story for pharma?) .
In the complex landscape of DHS, addressing these unique challenges is not just advisable — it's indispensable for PharmaCos looking to make a profound impact and navigate the digital health solution terrain with finesse.
Experience-based DHS guidelines for success
Developing digital health solutions demands a nuanced approach, one that we have refined through numerous successful projects. Drawing on our experiences, we've distilled a set of strategic guidelines tailored specifically for DHS development.
-
Empathy-driven design: User-centric DHS prototyping
The design thinking approach in digital health is a user-centric, iterative process involving understanding user needs, generating innovative ideas, and rapid prototyping and testing. It ensures active involvement of potential users, including HCPs, patients, and caregivers, from problem discovery to testing, iteration, and implementation. This approach demands a cross-functional team: strategists shape the solution's value proposition, medical and legal advisors ensure compliance, and user experience designers pinpoint pain points and design, test, and refine the solution. Dermanostic, a skincare telemedicine startup, serves as a prime example, engaging and iterating with customers early on, resulting in a solution finely attuned to their needs and preferences.
Our experience: For a rare disease DHS, involving specialist healthcare professionals and caregivers from the start enabled us to design user journeys, identify pain points, and develop effective solutions through iterative testing.
-
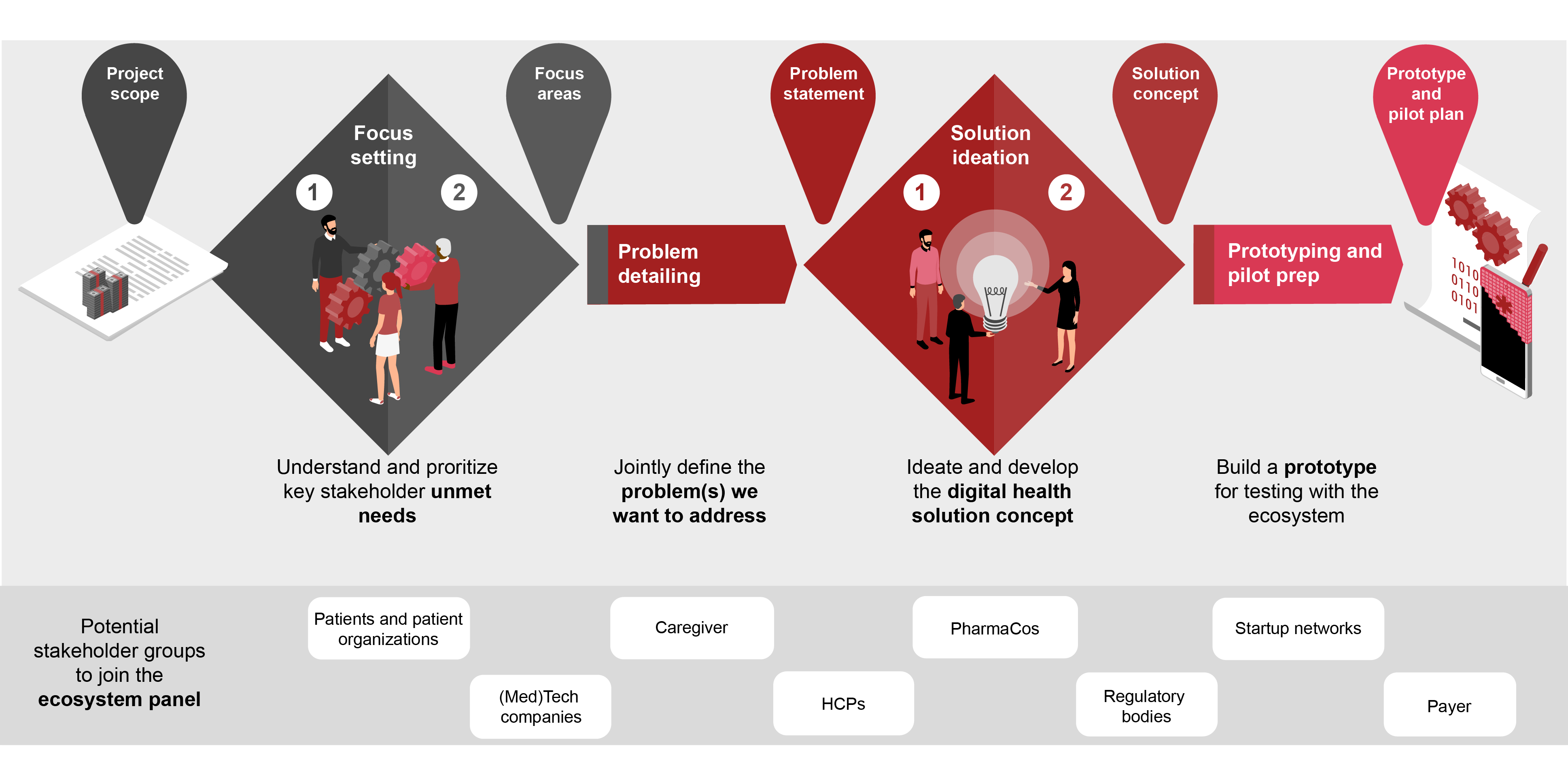
Ecosystem validation: Establishing market alignment
Validating DHS within the broader ecosystem is pivotal. An ecosystem panel, involving diverse stakeholders, ensures market suitability from multiple perspectives. Collaboration with tech companies, patient organizations, and payers not only expands networks but also fosters informal collaborations that may blossom into formal partnerships. In addition, this approach acknowledges the challenges of neutrality and Pharma ownership. The inclusion of patients and diverse other stakeholders in the panel fosters an end-to-end (E2E) perspective and cross-sector collaboration, leading to higher neutrality of the solution.
As exemplified by Doctolib, a pioneer in digital appointment booking, this approach broadens networks, bolsters credibility within the ecosystem, and confirms the solution's alignment with the broader healthcare landscape.
Our experience: After the initial ideas were captured during the project, tech companies, payers and others worked together to identify an even broader range of ideas and shaped them into meaningful concepts. They also supported judgements on feasibility, e.g., from a technology and regulatory perspective. -
Building trust: Neutral branding and credibility
In the pharmaceuticals and life science industry, the digital health solutions that thrive are those trusted by key opinion leaders, HCPs, caregivers, and patients. Brand trust is arguably one of the most valuable intangible assets. Brand trust creates loyalty, builds advocacy, and drives additional users. Often, PharmaCo-branded solutions achieve the opposite, to the detriment of their success. Branding that supports a digital health solution should instead underscore its PharmaCo neutrality and emphasize tools, content and processes vetted and co-created by key opinion leaders and solution users.
Our experience: HCPs, caregivers and patients clearly voiced the view that PharmaCo branding would undermine the credibility of the solution, since it would evoke the impression that it was developed to better position the PharmaCo and its products. Accordingly, we chose a neutral branding that highlights the partners, such as key opinion leaders and caregiver associations, to evoke trust from the solution’s users. -
Iterative business model validation: Ensuring growth
Generally, clarity on the value levers of a DHS and any expected revenues and costs - including the underlying assumptions - should increase over the course of DHS development. A clear value case is also important to ensure continuous support from the PharmaCo’s management and development partners. For a PharmaCo, a DHS can have significant scalability potential to other therapeutic areas, which should be reflected in the business model discussions. As the development progresses, it is essential to determine the expected remaining development and run costs, as well as the expected realistic revenues, e.g., through reimbursement or increased drug adherence. As demonstrated by Avi Medical, a pioneer in hybrid next-gen GP practices that is slowly growing its practice network and offering, an incremental approach ensures long-term success.
Our experience: By developing clear value propositions for each user group and partner, we created hypotheses that were validated over time, ensuring the business model's alignment with the evolving Digital Health landscapes. -
Design with the data strategy in mind
Data from DHS can be useful along a PharmaCo’s value chain in many ways, — powering clinical trials, real-world evidence, market research, and pharmacovigilance. An early, data-savvy strategy can shape and secure a digital health solution's value proposition. Prioritizing user-friendly, compliant, and safe data collection is a key driver for acceptance and buy-in. As illustrated by Qualifyze, a pioneer in centralized pharma audits with a business model built around their data, this strategic approach ensures that the data generated is not only valuable but also aligns seamlessly with the overall goals of the digital health solution.
Our experience: After the high-level concept had been established, on the one hand, we created transparency on the data that could be useful for a PharmaCo and various ecosystem stakeholders. On the other hand, technical experts and HCPs helped to shape the DHS concept from a functional perspective, to ensure that the data most valuable for users will be collected in a reliable and trusted manner. Fusing both sides results in a DHS that provides highly valuable data for all stakeholders.
Taking action: Where to begin
Digital innovators can accelerate their DHS development successfully by following these five steps:
- 1Identify a cause worth fighting for. Any DHS development should start with clear objectives for the PharmaCo, an initial value proposition for all stakeholders involved, and a business model incl. budget outlook that is able to secure initial backing and provides a promising outlook.
- 2Find and leverage the existing assets within your organization. Often, clients have existing development teams, previous DHS with similar components, documented user journeys and other fundamental elements that can accelerate the development.
- 3Define a thought-out development roadmap from ideation to prototyping and including the (human) resources required. Often, clients have existing development teams, previous DHS with similar components, documented user journeys and other fundamental elements that can accelerate the development.
- 4Involve potential users and further ecosystem stakeholders from the start. Before the development of a user-centric DHS can begin, a set of potential users and partners needs to be identified, e.g., to develop validated user journeys and pain points.
- 5Optionally, partner with an experienced third party. Depending on the experience in your organization and team, getting an experienced third-party partner on board that can guide you through the DHS development can make the difference between failure and success.
DH solutions are a key stepping stone to improve quality of life for patients, increase the efficacy of healthcare systems, and positively impact healthcare system organization. By applying the five recommendations in our guidelines, digital innovators can move the needle on successful DHS development.
Antonia Foeller also contributed to this report.
Contact us



